Causes of Antibiotic Resistance
To understand the causes of antibiotic resistance, we need to know the general idea about antibiotics and how they work. This article
aims to understand the action of antibiotics, causes of antibiotic resistance
and its consequences.
1. Antibiotics
Antibiotics are essential substances used to combat
bacterial infections across various medical conditions such as tuberculosis,
urinary tract infections, sore throat, skin infections etc.
2. How Antibiotics Work
Antibiotics act by inhibiting vital cellular processes
within bacteria, leading to their death.
For example, most prescribed antibiotics i.e. β-lactams inhibits
enzymes necessary for bacterial cell wall synthesis, resulting in rupture of
bacterial cells by increased internal pressure.
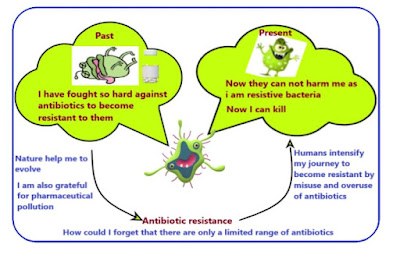
3. Understanding Antibiotic Resistance: Definition
Antibiotic resistance refers to the evolutionary adaptation
of bacteria to withstand the effects of antibiotics, rendering these drugs
ineffective in eliminating bacterial infections.
Antibiotic resistance is a natural process which is intensified
by human activities.
4. Antibiotic Resistant bacteria
Antibiotic-resistant bacteria are strains that have evolved
mechanisms to survive in the presence of antibiotics, rendering the drugs
ineffective against them.
5. Causes of Antibiotic Resistance
The causes of antibiotic resistance stems from natural
evolutionary processes, human-induced factors and non-availability of new class
of antibiotics.
5.1 Natural evolution
Antibiotic resistance arises from the fundamental desire to
survive inherent in all living organisms, including bacteria. Just as a person
instinctively repairs a leaky roof during a storm to protect himself, bacteria
have evolved over time to develop mechanisms that counteract the effects of
antibiotics.
So, instead of getting killed by these drugs, bacteria adapt
and develop resistance, making antibiotics ineffective against them. This
innate survival instinct drives bacteria to evolve and respond to the threats
posed by antibiotics, posing a significant challenge to our ability to
effectively combat bacterial infections.
5.2 Human activities
The overuse and misuse of antibiotics has increased since
their discovery, which is further intensified by their widespread use without
proper prescription.
Additionally, agricultural and pharmaceutical wastes from various sources including farms, hospitals, industries, and homes seep directly into environmental ecosystems such as landfills and water bodies. So, bacteria found in water bodies and landfills comes in contact with the antibiotics which simply escalate the process of antibiotic resistance. This in turn increase the spread of antibiotic resistance in bacteria, posing a serious threat to public health and environmental well-being.
Also, not adhering to the prescribed course of antibiotics
can contribute significantly to the development of antibiotic resistance. When
antibiotics are not taken as directed, such as skipping doses or stopping
treatment prematurely once symptoms improve, it creates an environment where
some bacteria survive exposure to the drug. These surviving bacteria, which may
be the more resilient or resistant ones within the population, can then
multiply and spread, potentially leading to the emergence of antibiotic-resistant
strains.
5.3 Non-availability of new class of antibiotics
The current situation regarding antibiotic availability is
concerning due to the limited variety of antibiotic classes, with a prominent
example being the β-lactam based antibiotics. These antibiotics, which include
penicillins and cephalosporins, have been widely used for decades. However,
their effectiveness against bacteria is increasingly compromised as many
bacterial strains have developed resistance to them.
This resistance arises from various factors, such as over prescription of β-lactam antibiotics, which can occur due to factors like
cost, ease of production, and accessibility. Bacteria adapt and evolve in
response to this constant exposure, leading to the emergence of strains that
are resilient to these drugs.
To address this issue, there is an urgent need for the
development of new classes of antibiotics with different mechanisms of action.
These novel drugs would offer alternative ways to combat bacterial infections,
reducing the reliance on β-lactam antibiotics and potentially overcoming
resistance issues.
So overall evolution in bacteria, overuse and misuse of
antibiotics and non-availability of new antibiotics are major causes of antibiotic
resistance.
6. Consequences of Antibiotic Resistance
The consequences of antibiotic resistance are multifaceted
including
·
Prolonged treatment duration
·
Escalating healthcare costs
·
Increased mortality rates
Imagine a time when antibiotics were non-existent, and
entire populations faced extinction in the wake of bacterial infections.
Infection with deadly diseases spelled certain death for individuals, with no
hope for a cure. Now, envision a future where antibiotics lose their efficacy
against bacterial infections, leaving scientists tirelessly seeking alternative
treatment approaches.
The escalating costs of antibiotics, driven by
substantial research and development investments, coupled with their dwindling
effectiveness over time due to antibiotic resistance, render pharmaceutical
industries unable to recoup their investments.
7. Conclusion
The rise of antibiotic resistance poses a formidable challenge to global public health, necessitating concerted efforts to mitigate its impact. Through prudent antibiotic stewardship, rigorous surveillance, and the pursuit of innovative therapeutic strategies, we can endeavor to safeguard the efficacy of antibiotics and limit the danger of antibiotic resistance.